Maimonides Health delivers a comprehensive model of preventive cardiology, supporting patients across their lifespan with evidence-driven strategies that reduce the burden of cardiovascular disease.
“Prevention starts as soon as we uncover a patient’s risk,” says Inna Nelipovich, MD, cardiologist at Maimonides. “We treat primary risks, we treat secondary risk factors, and we guide people on the path to living longer, healthier lives.”
While providers often refer only after the cardiovascular disease have progressed, Dr. Nelipovich stresses that early attention from a specialist improves long-term outcomes.
“Early cardiovascular risk detection becomes important when patients present with elevated blood pressure, high cholesterol, elevated blood glucose, autoimmune conditions, kidney disease, or vascular symptoms,” she said. “A single identified risk factor is enough reason to connect a patient to more in-depth screening.”
Dr. Nelipovich also recommends a referral for anyone with a family history that warrants earlier screening, especially if they have a male relative who develops heart disease before the age of 60 or a female relative before the age of 65.
For practices seeking a trusted Brooklyn cardiologist referral, Maimonides offers rapid access, coordinated management, and streamlined communication with the referring provider.
Team-Based Model That Meets Brooklyn’s Needs
Brooklyn’s demographic mix brings varied genetic backgrounds, socioeconomic stresses, and inconsistent access to care—all factors that can complicate cardiovascular health and outcomes.
“Many of our patients face economic stress and limited access to care. Sometimes we are the first doctors they see in years. We also care for immigrants from all over the world, which means different genetic risk factors,” Dr. Nelipovich explains.
Preventive services connect directly with cardiology, primary care, women’s health, nephrology, rheumatology, and endocrine and metabolic services. Specialists share information through a unified system and a campus layout that strengthens care coordination. “It helps that all these subspecialties are located in the same building,” she says. “A patient can move between floors and receive coordinated input from cardiology, endocrinology, weight management, and women’s health without delay.”
Neurology also plays a key role, since stroke risk factors often overlap with cardiovascular risks, especially when arrhythmias are suspected.
The vascular surgery team contributes as well, given that nearly 30% of patients with peripheral vascular disease also have coronary disease. And for patients born with congenital heart disease, Maimonides coordinates lifelong prevention through a transition from pediatric cardiology to adult cardiovascular care.
Diagnostic Tools Strengthen Early Recognition
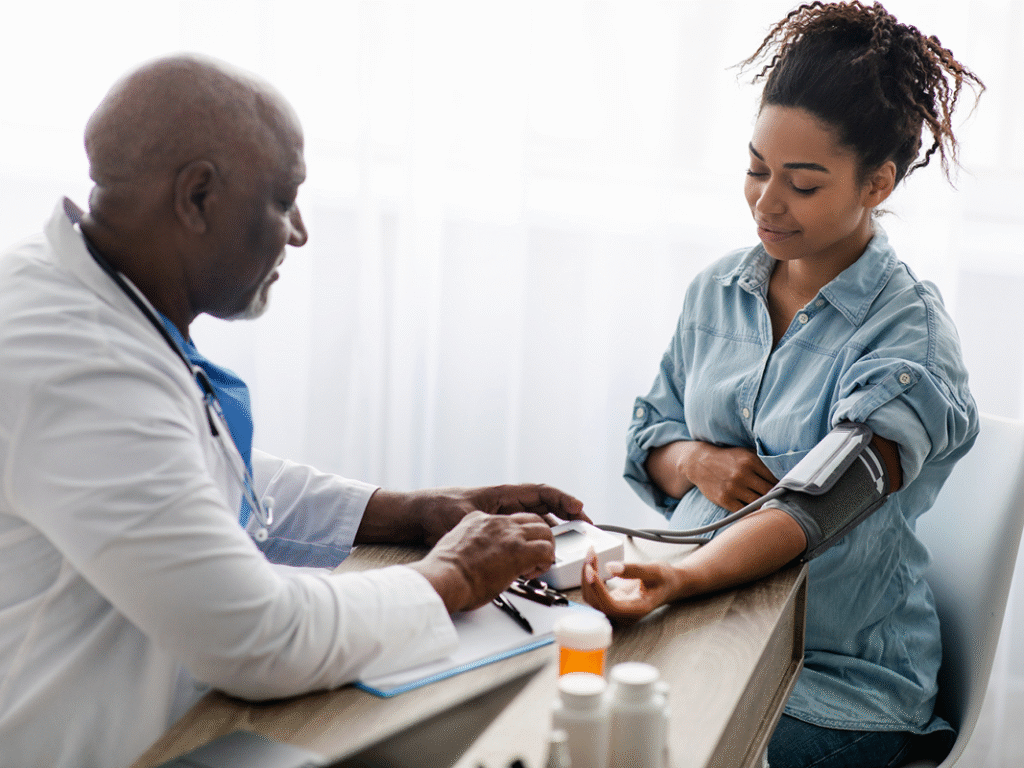
The program uses foundational and advanced diagnostic tools to support cardiovascular risk reduction and detect early disease. “The simplest tool is still the physical exam,” Dr. Nelipovich says. “Blood pressure measurements are essential because hypertension often goes undetected for years.”
Other diagnostic approaches include:
- Electrocardiograms
- Echocardiograms to evaluate cardiac structure and valve function
- Holter and event monitors for rhythm assessment
- Loop recorders for long-term arrhythmia surveillance
- Stress echocardiography
- Coronary calcium scoring
- Coronary CT angiography to assess plaque and congenital anatomy
- Cardiac MRI
- Nuclear stress testing
“We make sure every test is appropriate and feasible,” she says. “Prevention must be cost-effective while providing the most benefits to patients.”
Weight Management as a Cardiovascular Intervention
Dr. Nelipovich places a strong emphasis on the link between weight management and heart disease. “Obesity, metabolic syndrome, and heart disease often overlap and intensify long-term cardiovascular outcomes. We know metabolic syndrome is associated with heart disease,” she says. “By treating obesity, we can reduce cardiovascular risk factors by a significant amount. When a patient loses weight, they move better, feel better, and get better control of their diabetes, elevated cholesterol, hypertension, sleep apnea, atrial fibrillation, and heart failure.”
Maimonides’ program collaborates with Maimonides Weight Management Center and endocrinology, especially as GLP-1 medications reshape obesity and metabolic care. “New medications for weight loss do more than reduce weight,” she explains. “They also control diabetes and lower future risk of heart attack and stroke.”
This coordinated model eliminates siloed care plan management. Patients see multiple specialists within the same clinical environment, and care plans remain tightly linked.
Women’s Cardiovascular Risk
Women’s cardiovascular symptoms rarely follow the patterns seen in men.
“For women, a lot of times prevention starts at a much younger age,” says Dr. Nelipovich. Often, cardiac risks appearduring pregnancy, when blood pressure or glucose elevations reveal early cardiovascular stress. These signals warrantearlier screening and referral. High-risk obstetrics team refers pregnant women directly to cardiology for monitoring, and postpartum follow-up ensures continued screening for long-term risk. After childbirth, preeclampsia, gestational hypertension and gestational diabetes continue to influence long-term risk. She encourages providers taking care of pregnant patients to watch for:
- Persistent fatigue, unusual extremity swelling, severe headaches, palpitations, jaw or neck pain, and shortness of breath
- Subtle symptoms that mimic GI or musculoskeletal issues
Integration with Heart Failure Treatment and Cardiac Rehabilitation
Within Maimonides’ comprehensive Heart & Vascular Institute, preventive cardiology links directly to specialized programs such as Maimonides’ Advanced Heart Failure Center. “We are fortunate to have excellent heart failure specialists,” Dr. Nelipovich says. “They raise the level of care for patients already living with the condition.”
Maimonides’ cardiac rehabilitation program strengthens recovery after heart attacks and cardiac surgery, providing monitored exercise and a structured progression back to daily function. “Patients often fear exertion after a heart attack or surgery,” she says. “Cardiac rehab gives them the confidence to start walking and exercising again as the monitored setting reassures safety and leads to real physical progress.”
Continuity Across Interventional and Electrophysiology Care
Preventive care remains the priority, even for patients who already live with coronary artery disease or rhythm disorders. Many individuals reach Maimonides once disease takes hold, or after years of silent risk once symptoms escalate, and they often need acute treatment in interventional cardiology or electrophysiology. Our interventional services are ready 24 hours a day to tread heart attacks and open blockages with PCI and stenting.
Our electrophysiologists manage the full spectrum of rhythm conditions, workup for syncope, or stroke-related rhythm concerns. We offer a range of arrhythmia ablations, pacemakers, defibrillators/ICDs, and loop recorders on-site.
Yet these patients still benefit from the same preventive guidance—nutrition support, weight management, exercise counseling, and ongoing risk-factor control—that anchors the program. Prevention does not end once a device is placed or a stent is deployed; it remains essential for protecting long-term heart health and improving outcomes across the continuum of care.
Guidance for Referring Providers
Dr. Nelipovich recommends referrals when patients present with:
- Atypical symptoms that raise concern
- Autoimmune disease or kidney disease
- Diabetes mellitus, especially with poor control
- Family history of cardiovascular disease
- Fluctuating or uncontrolled blood pressure
- Peripheral vascular disease
- Persistent hyperlipidemia
- Pregnancy-related hypertensive or metabolic diagnoses
- History of Preeclampsia with prior pregnancies
“Referring earlier helps us prevent heart attacks, strokes, arrhythmias, and long-term heart failure,” she says. “A proper identification of risk factors is key.”
Learn more about Maimonides Heart & Vascular Institute. To refer a patient or request a consultation with the Maimonides preventive cardiology team, call 718-HRT-BEAT (718-478-2328).