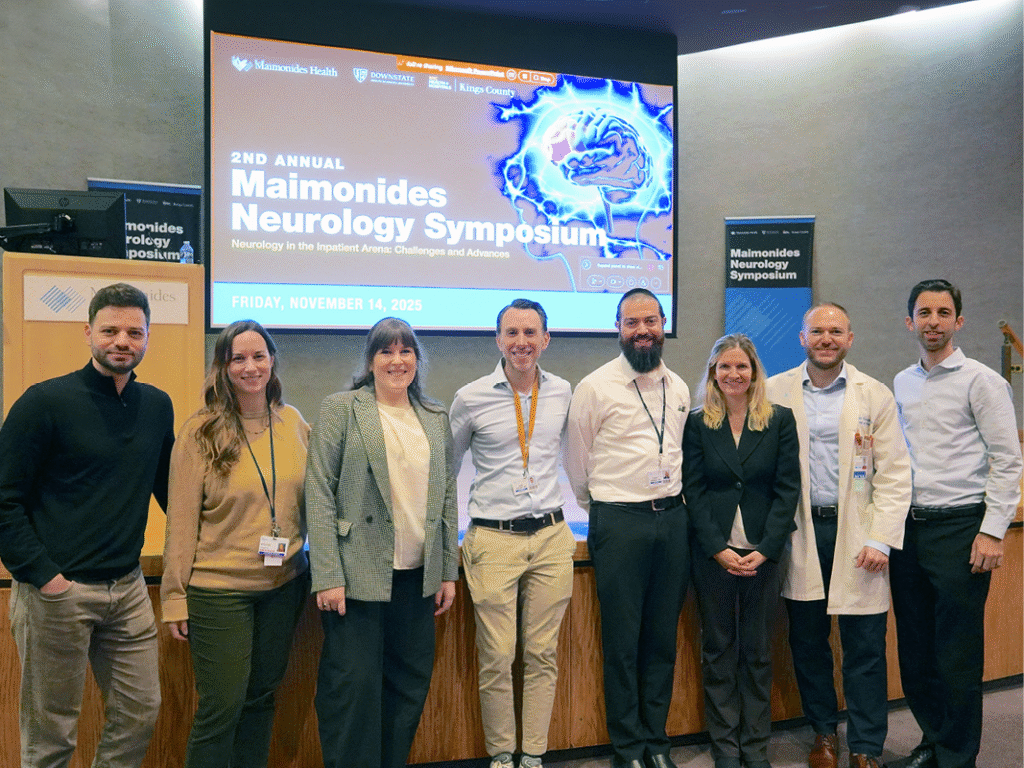
On Friday, November 14, Maimonides Neurosciences Institute, Brooklyn Neuroscience Center at NYC Health + Hospitals/Kings County, and SUNY Downstate Health Sciences University Department of Neurology held the second annual Maimonides Neurology Symposium.
Organized by Nuri Jacoby, MD, Vice Chair of Neurology at Maimonides Medical Center and Associate Professor of Clinical Neurology at SUNY Downstate Health Sciences University, the symposium drew more than 400 participants who attended remotely and in-person.
Challenges and Advances in Inpatient Neurology
While last year’s symposium centered around advancements across neurologic subspecialties, including multiple sclerosis, epilepsy, and Alzheimer’s disease care, this year’s focus was on inpatient neurology outside of the umbrella of stroke care.
“When patients with primary or secondary neurologic symptoms are admitted into the hospital—whether for acute care, critical care, surgery, or other areas—they often have challenging presentations and conditions that require collaborative care from physicians, surgeons, advanced practice providers, and nurses across multiple disciplines,” said Dr. Jacoby.
Dr. Jacoby worked closely with Maimonides neurohospitalists, especially Elizabeth Chernyak, MD, to develop the day’s programming with the goal of creating accessible takeaways for real-world practice for those attending across various clinical backgrounds.
Neurologic Complications of Cancer Immunotherapy
“Neurologic Complications of Cancer Immunotherapy” was presented by Bianca Santomasso, MD, Assistant Attending Neuro-oncologist at Memorial Sloan Kettering Cancer Center. Dr. Santomasso is one of the world’s foremost experts on this new area of neurology that has emerged in the medical literature over the past five to 10 years.
“Monoclonal antibodies called immune checkpoint inhibitors were developed to prevent cancer cells from upregulating immune system checkpoints to escape anti-tumor surveillance,” said Dr. Santomasso. “However, neurologic immune-related adverse events have proved an increasing challenge as these immunotherapies become more widespread, affecting up to 50% of patients treated with immune checkpoint inhibitors. These adverse events are diverse, with varied presentations, affecting both the central and peripheral nervous systems.”
According to Dr. Santomasso, these neurologic immune-related adverse events usually occur within the first 12 months of starting immunotherapy treatments, with the most severe reactions becoming apparent within the first three months. It can present as myasthenia gravis, myositis, peripheral neuropathy, encephalomyelitis, and meningitis; diagnosis requires electrodiagnostic testing, cerebrospinal fluid evaluation, lab testing, and MRI. In rare cases, delayed diagnoses can lead to fatalities, but early recognition and treatment can lead to better patient outcomes.
Dr. Santomasso advised on general principles of neurologic immune-related adverse event management dependent on severity. Currently, the mainstay of treatment for most types of neurotoxicity is corticosteroids. As this field develops, better understanding of the pathogenesis of these toxicities will lead to more tailored management.
Preventing and Treating Inpatient Delirium
Daniel Shalev, MD, Assistant Professor of Medicine and Medicine in Psychiatry, Weill Cornell Medicine, presented on “Psychiatric Dilemmas in Inpatient Neurology,” guiding attendees through the process of evidence-based delirium assessment, treatment, and prevention strategies.
“Long-term outcomes of delirium include cognitive impairment, poor functional outcomes, decreased quality of life, dementia, longer inpatient stay, increased readmissions, and greater risk of mortality,” said Dr. Shalev. “While we can’tmitigate every risk factor, many are modifiable. Utilizing multicomponent, nonpharmalogic approaches like management of nutrition, hydration, seizures, infections and infection risk, sleep quality, and mobilization can effectively prevent delirium.”
Among the delirium treatment strategies Dr. Shalev discussed was pharmacotherapy for psychiatric symptoms, as well as antipsychotic medications to manage agitation and delirium. These should not be used as preventive measures,according to Dr. Shalev, as they are not shown to reduce duration of delirium, improve distressing symptoms, improve outcomes, or reduce mortality. In general, he also advised that benzodiazepines can cause or worsen delirium, and should only be utilized in specific cases, such as patients receiving palliative care.
Acute Neuropathies and Guillain-Barre Syndrome
Dr. Jacoby’s presentation, “Acute Neuropathies – Is It Always Guillain-Barre?” was inspired by several complicated seenthis year at Maimonides. The presentation explored causes of acute neuropathies—including Guillain-Barre Syndrome, vasculitic conditions, nutritional deficiencies, and infectious diseases like Lyme, HIV, or hepatitis—as well as the diagnostic processes to identify them.
He discussed treatment protocols for Guillain-Barre, including guidance on intravenous immunoglobulin administration within two weeks from onset of symptoms, and only in a single dose to minimize risk of serious adverse events.
“Guillain-Barre is well-known to many providers, and can be treated by hospitalists, critical care specialists, and others in addition to neurologists,” said Dr. Jacoby. “From the neurology side, it is very important to help familiarize care providers with the mimics and lesser-known causes of acute neuropathies, as the necessary treatment and management differs greatly depending on the cause.”
Dr. Jacoby discussed emerging diagnostic techniques to confirm Guillain-Barre cases, like elevated neurofilament light chain (NfL) levels. New treatments are also on the horizon for Guillain-Barre, including ANX005, a C1q inhibitor that has been found to improve GBS-disability score and muscle strength and reduce NfL chain levels.
Recognizing Neuroinfectious Diseases
Yaacov Anziska, MD, Associate Professor of Clinical Neurology and Neuromuscular Division Chief, SUNY Downstate Health Sciences University, presented “Cases in Neuroinfectious Diseases.” Like Dr. Jacoby, Dr. Anziska also used real-world examples of patients here in Brooklyn, walking attendees through testing processes and diagnosis of patients who present with neurologic symptoms like encephalitis.
Dr. Anziska began the presentation with a discussion of the effects of climate change on overall infectious disease risk.
“The warming climate is allowing bacteria and viruses to spread more easily to new geographic locations, and climate-related hazards can enhance pathogens and weaken humans’ ability to cope,” said Dr. Anziska. “For instance, studies suggest that rising temperatures can help viruses and fungal pathogens become more resistant to heat, resulting in increased disease severity as pathogens become able to adapt to fever in the human body.”
In the diagnostic process for neurologic symptoms like encephalitis, seizures, sensory changes, weakness, coordination issues, and stiff neck, it is critical to consider every patient’s potential infectious disease risk factors, especially in a highly globally connected city such as New York. Providers should be aware of patients’ medical history, travel history, and potential exposures to food-related and environmental exposures, as well as exposures to STIs and even infections that can develop in fetuses during pregnancy.
The talk underscored the importance of having a wide knowledge of potential diagnoses in this area, with applications for medicine, neurology, emergency medicine, and other disciplines.
Critical Care and Neuropalliative Care for Neurology Patients
Other topics covered in this year’s symposium included “Topics in Critical Care EEG” from Susanna O’Kula, MD, Attending Physician, Neurology, Maimonides Medical Center; “Navigating Goals of Care in the Inpatient Setting” from Eileen Harrigan, MD, Clinical Assistant Professor of Neurology, NYU Grossman School of Medicine; and “Neuroprognostication Post Cardiac Arrest” from Darya Khazanova, MD, Attending Physician, Neurology, Maimonides Medical Center.
These discussions centered around a common theme of guidance for best practices in decision-making for providers across the often-difficult topics and dilemmas of helping patients in critical or terminal situations.
Additionally, Dr. Anziska and Christian Amlang, MD, Attending Physician, Neurology, Maimonides Medical Center, led an exclusive in-person panel: “A Multidisciplinary Evaluation of Gait.” The panel featured a live neurologic examination demo with two Maimonides Neurosciences Institute patients.
Providing Opportunities for Academic Growth
For its second year, the Maimonides Neurology Symposium brought a significant resource to regional neurology care, uniting diverse medical professionals, from neurologists to emergency medicine practitioners.
“This symposium is really a unique opportunity to bring together a lot of different speakers and types of clinicians, to stay updated on the latest advancements in neurology and to foster collaboration among healthcare providers,” said Dr. Jacoby.
“As one of the largest teaching hospitals in the city and the largest hospital in Brooklyn, one of our central goals is to provide educational opportunities to our medical peers in the community, ensuring that local clinicians remain at the forefront of neurological care.”
Learn more about the annual Neurology Symposium and neurology care at Maimonides. To refer a patient or schedule an appointment, call 718-283-7470.