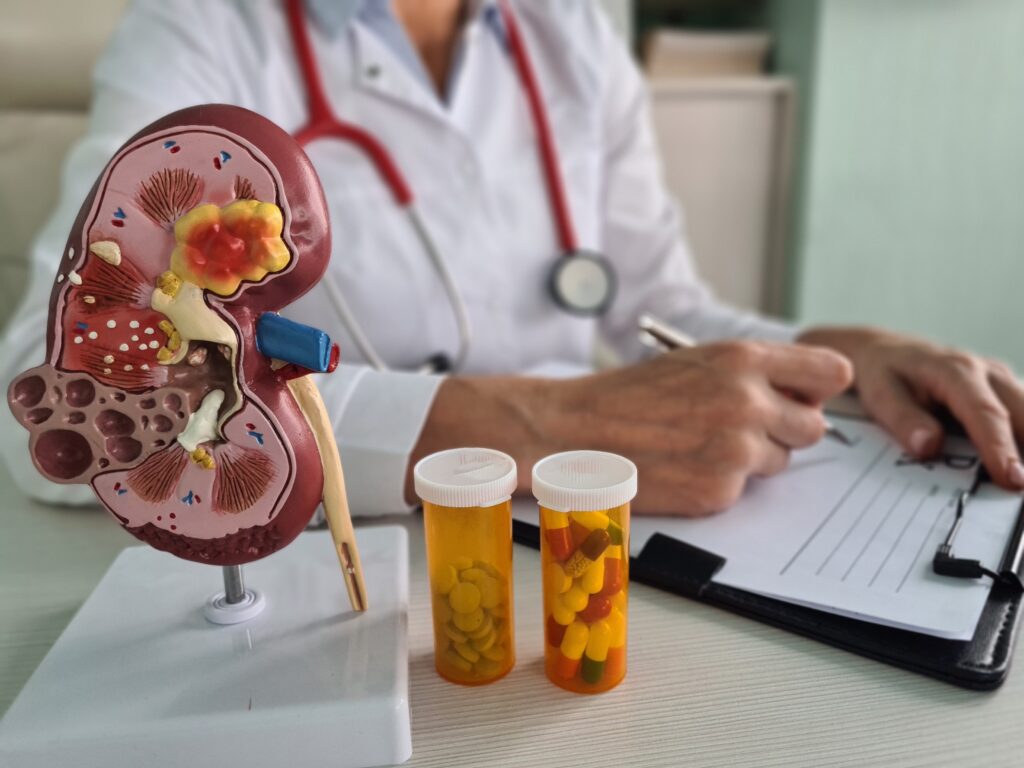
For many patients with kidney disease, including the roughly 2 million in the New York metro area estimated to be affected by chronic kidney disease (CKD)1, nephrology care may seem synonymous with dialysis. Recent advances in treatment, however, are expanding the scope of nephrology care, giving patients and providers more effective options, especially when these issues are caught early on.
At Maimonides’ Division of Nephrology, clinicians have long been dedicated to providing strong outpatient services for patients with kidney disease, setting their practice apart among a field of medicine that is practiced largely through inpatient care.
“Maimonides is unique in our strength and quality of outpatient nephrology services in this area,” says Sheldon Greenberg, MD, Director of Nephrology at Maimonides. “For years, we’ve devoted ourselves to building up our outpatient nephrology practice and caring for patients with CKD to slow down progression.”
Revolutionary Treatments Effectively Preserve Kidney Function
In recent years, many treatments have emerged that have transformed the management of CKD like diabetic nephropathy, polycystic kidney disease and lupus nephritis.
SGLT2 (sodium-glucose cotransporter-2) inhibitors are one example. Originally developed as a treatment for type 2 diabetes, several are now approved by the FDA to treat CKD in patients with or without diabetes.
“SGLT2 inhibitors have been shown in several studies over the past three years to stabilize and slow down the progression of CKD, which previously had very limited options in terms of stabilization,” says Hillary Grainer, DO, attending physician in the Division of Nephrology at Maimonides. “They lower blood pressure and blood sugar, preventing kidney damage, and decrease the amount of protein in urine, a hallmark of CKD.”
Along with ACE inhibitors and ARBs, the long-available blood pressure and CKD treatments, finerenone is another treatment available to patients that has been shown to slow progression of CKD. Finerenone has emerged within the past five years as a safe, effective therapy targeted specifically toward patients with CKD at any stage, and has been available to Maimonides patients for several years.
Along with ACE inhibitors and ARBs, medications that have long been used to treat blood pressure and slow CKD, finerenone has also been approved to slow progression of CKD. Finerenone has emerged within the past five years as a safe, effective therapy targeted specifically toward patients with diabetic nephropathy at any stage, including patients with heart disease, and has been available to Maimonides patients for several years.
Targeted Therapies for Specific Renal Diseases
For years, nephrologists had limited treatments for polycystic kidney disease. Now, tolvaptan has emerged, a drug that directly decreases the size of cysts on the kidneys. Maimonides nephrologists have quickly become experienced in stabilizing polycystic kidney disease with this treatment, which is not very well known even within the nephrology community.
“Tolvaptan is the first medication shown to decrease the size of the cysts, in addition to blood pressure medications,” said Dr. Grainer. “It is well suited to younger patients, below the age of 50, who retain the most residual renal function. Sides effects can include liver enzyme elevation, so we provide monthly liver enzyme monitoring to ensure these medications are safe and effective for every patient.”
Patients with systemic lupus erythematosus are at high risk of developing lupus nephritis, a condition that can lead to kidney failure when left unmanaged. According to Dr. Greenberg, two medications approved within the last five years, belimumab and voclosporin, are being proven to effectively treat lupus nephritis, decreasing proteinuria for patients. For several years, Dr. Greenberg and other Maimonides nephrologists have been utilizing these medications to help lupus nephritis patients manage their conditions and gain better outcomes.
“We’re really focusing on slowing down progression of disease and stabilizing kidney function,” says Dr. Greenberg. “If you didn’t have the benefit of these medications and expertise, these kidney diseases would progress until patients end up on dialysis. Now, patients can live years longer off dialysis, majorly changing their quality of life for the better.”
Identifying and Avoiding Complications
Appropriate management of kidney diseases can help patients avoid complications they may experience as a result of the disease itself or suboptimal treatment methods. Patients with CKD often have systemic, multiorgan problems, which Maimonides nephrologists are well-versed in navigating. It is important for patients to receive these assessments from a specialist, as not all internists retain a consistent awareness of the unique systemic effects of kidney disease.
“Complications need to be sought after and identified, as they are often present long before dialysis and aren’t caught in a routine blood test,” says Dr. Grainer.
These complications can be treated medically and through dietary changes. An example is electrolyte imbalances, which can cause cardiac issues for patients. Patients may require sodium, potassium, calcium, or phosphorus restriction in their diet, increased water intake, or medical therapies to prevent adverse effects on the heart.
Additionally, when each patient sees a Maimonides nephrologist, their entire regimen of medications is evaluated for safety and correct dosage considering the unique physiology of kidney disease.
“We evaluate medications because even those that are ordinarily beneficial can actually harm a CKD patient,” says Dr. Greenberg. “This is because the kidney may eliminate certain medications, and because the kidney is now weaker, the medications can accumulate. That may not be known to all physicians. Certain drug interactions may also cause greater harm to the kidneys. For example, if a person has CKD or hypertension and is taking an NSAID like ibuprofen, even though it’s a common, over-the-counter medication, it can cause significant damage to the kidneys. Many patients don’t receive the counseling necessary to have that awareness, until they come to our practice.”
Even treatments targeted toward kidney disease can potentially exacerbate worsening renal function. ACE inhibitors or ARBs, for example, can lower blood pressure, but can increase potassium levels in some patients, so expert monitoring is necessary in both the diagnostic and treatment stages.
Early Identification of Kidney Disease is Critical to Slowing Progression
Most individuals with CKD are unaware of their condition, which is why asymptomatic screening is critical. With these comprehensive services available, conscientious primary care is key to accessing early diagnosis and securing the best chances of stabilization of kidney function.
The most common methods of screening for CKD are blood and urine testing. Blood testing for creatinine can detect kidney disease, but it should not be the first line of defense in screening.
“What is often not well-known about creatinine testing is that once the creatinine rises above normal, already 50% of the kidneys’ function could be damaged,” says Dr. Greenberg. “By the point at which up to 40% of the kidney has incurred damage, the creatinine test may still be normal. Once it rises to the point of being just slightly abnormal, the damage will already be significant.”
All well visits should include routine urine tests to screen for albuminuria, or the presence of protein in urine. A significant amount of protein in the urine is an indicator that a patient should begin to be evaluated for kidney disease – even if blood tests show that creatinine is normal.
Aside from albuminuria or elevated creatinine, if potassium or sodium levels are elevated, those are also signs to refer a patient to a nephrologist. Another red flag is high blood pressure that is difficult to treat; nephrology specialists can determine if the elevated blood pressure is being caused by secondary causes related to renal function.
“Early on is the best time to diagnose kidney disease,” says Dr. Greenberg. “The earlier these problems are identified, the more likely is that patients will be able to be cured or that their condition will be stabilized.”
For more information on nephrology care at Maimonides, visit https://maimo.org/treatments-care/nephrology/. To refer a patient, call (718) 283-7908.
1: https://www.kidney.org/greater-new-york-ending-disparities-and-inequities-ckd-leadership-summit#:~:text=Approximately%202%2C220%2C000%20adults%20in%20Greater,adults%20are%20aware%20of%20it.