Summary
Robotic surgery has been a game changer in the orthopedic field. Dr. Jason Wong discusses the latest technology in joint replacement surgery using robotic surgery. Maimonides Medical Center was named among America’s Top 100 Hospitals for Orthopedic Surgery (Healthgrades, 2022).
Listen on Spotify Listen on Apple Podcasts Listen on Google Podcasts
Transcript
Amanda Wilde (Host): Robotic surgery has been a game changer. And today we’ll talk about the latest technology in joint replacement surgery with Dr. Jason Wong, orthopedic surgeon at Maimonides bone and joint center in Brooklyn.
Amanda Wilde (Host): This is Maimo Med Talk. I’m your host, Amanda Wilde. Dr. Wong, thank you so much for being here. What do you do at Maimonides? What is your medical specialty?
Dr Jason Wong: Hi. thanks for having me today, Amanda. I specialize in orthopedic surgery, and I do hip and knee replacements. That’s my subspecialty.
Amanda Wilde (Host): So you specialize in hip and knee replacement and, in your practice, have you seen a great deal of change in terms of technological advancement in treatment for knee and hip injuries?
Dr Jason Wong: Yeah, I think, for the most part, I do hip and knee replacements for people who have arthritis. So, not really an injury, but it’s more like a wear and tear phenomenon as they get older. I think, for what I do for a living, we named the hip and knee replacement world, things have changed a lot over the last 10 years. And we were able to decrease blood loss by giving them a special medication. We’re able to navigate the goal of going home discharge method compared to going to rehab back in the days. And, obviously the topic for today, the robotic part changed a lot of how we do hip and knee replacements for the last six, seven years now.
Amanda Wilde (Host): So, can you talk about how the traditional and the robotic surgery are different for hip and knee replacements?
Dr Jason Wong: Yeah, sure. I mean, overall, like when you are doing a conventional or traditional hip and knee replacement, you rely a lot on patient’s anatomy that we know based on historical data. We use a lot of eyeballing using our naked eyes to see how things are aligned and we try to do it that way for every single person. So basically, it’s a one-size-fits-all kind of thing or one-technique-fits-all kind of thing. But then, with the robotic surgery, we were able to scan the hips and knees of the patients before the surgery. And in that case, we know exactly the alignments for each individual patients. And in that sense, during the surgery, we have a better idea of each patient’s anatomy. But also, intraoperatively, we’re able to control what we exactly are doing instead of using the eyeball so much and things are much more accurate that way.
Amanda Wilde (Host): So way more accuracy is a clear advantage of robotic surgery. Who’s a candidate for this kind of surgery?
Dr Jason Wong: In fact, I think like all comers can be candidates for robotic surgery. We don’t really screen out patients between conventional and robotic. But that being said, we do have some criteria on what patients whether we can operate on safely, but it’s not secondary to robotic part versus the traditional part. Just overall, we have to medically optimize the patients before we do surgery, like in the world of hip and knee replacements because, at the end of the day, these are elective surgeries, so meaning that patient has to be healthy before they go through these kinds of surgeries.
Amanda Wilde (Host): They have to be healthy, but they also need a knee or hip replacement, which I think is fairly common, isn’t it? Is it common after a certain age?
Dr Jason Wong: Yeah. In fact, like there were studies that showed about 20% of patients over 60 years old have some kind of arthritis. And definitely, the trend of hip and knee replacement is going up on the rise because of populations getting healthier so they can live longer. However, the joints won’t hold up when they get old.
Amanda Wilde (Host): Right, right. Well, help me visualize what this robotic assistant looks like. I mean, are you actually performing surgery alongside some C-3PO type of being or Sonny from I, Robot? Or what is this robot?
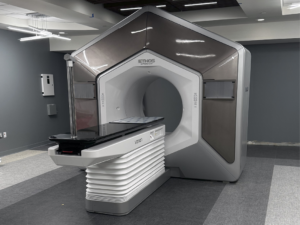
Dr Jason Wong: So the robot does not have a face. The robot is essentially like a robotic arm. So when we perform surgeries, for example, in hip surgery, we got to place a cup in a certain position or in total knees, we have to make about 10 to 12 bony cuts on the femur and tibia. The robotic arm incorporates the CT scan that we obtained before the surgery. And during the surgery, I would tell the robot exactly where this patient’s knee is by putting antennas and using registration protocol. Now, while I’m doing the cuts, the robot was able to incorporate the real time and the pre-scan data into their, whatever, their brain. And then while I’m doing the cuts, the robot would tell me, “Hey, don’t go too far. Let’s stop here. Let’s stay here. Let’s go a little further. Let’s raise your hand a little bit.” But all of these, we call haptics, are all designed by us before the surgery also, meaning that I set criteria for the robot before I do any part of the procedure. And then within that criteria that I set for a robot, the robot would tell me where I’m actually doing it, when to start, when to go.
Amanda Wilde (Host): So, it’s a tool that you’re operating, just like you would have used a scalpel in the old days.
Dr Jason Wong: Yes. It’s almost like a smart tool, so the scalpel can actually tell you, like, “Don’t cut too deep,” that kind of thing. But that being said, I wanted to emphasize, all this criteria, like what is considered deep or not deep, is still designed by me. Before the surgery, we went over every single parameters with the robots. But then interoperatively, when we’re doing it, the robots follow my criteria to tell me where I’m doing it, when to stop it, when to start.
Amanda Wilde (Host): So you really have to be an expert to program the robot exactly for each patient.
Dr Jason Wong: Yup. You really have to know the anatomy and to know the alignments and to have a sense of balancing of the knee before you can input those criteria.
Amanda Wilde (Host): So once you have done the surgery, how do you know it was successful?
Dr Jason Wong: So a couple of things, number one would be a radiographic picture. So after surgery, we all obtain what we call a postoperative x-ray. Obviously, you go look at the alignment of the components, making sure that they’re in good position. In fact, the robotic surgery or the studies have shown that we’re able to obtain an acceptable x-ray more often in robotic surgery than conventional method. So that’s one, radiographic outcome.
Secondly is clinical outcome. Is the patient feeling better? Is the patient feeling that the pain is less than how it was after the surgery. Now, obviously, we’re not talking about like two hours after surgery, because a patient will be having like the postoperative pain that’s because we cut through the knee and hips. But we’re talking about like two weeks, four weeks, six weeks data, and see if their pain improves significantly as the surgery pain wears off, so that’s number two, which is the pain level.
And then the third thing will be how did they go back to normal activities? Like for example, you ask them how much stairs can you climb six weeks post-op compared to two weeks pre-op? Or asking about, “Did you go back to work? How’s your work doing now?” Just more activities of daily living, that kind of stuff, to see if the surgery is successful.
Amanda Wilde (Host): Yeah. What I was just going to ask is what is the recovery process after a robotic surgery? And it sounds like it’s a few weeks. In two weeks, there’s a milestone and maybe six weeks, you
Dr Jason Wong: Yeah.
Amanda Wilde (Host): milestone.
Dr Jason Wong: Yeah, that’s absolutely correct. So after the surgery’s over, what happens to the patients, usually they will be evaluated by a therapist in the hospital. If they were clear, meaning that they achieved some milestones on post-op day zero, they can actually go home the same day. When they go home, we send home with them our visiting nurse, our visiting therapist. They would get therapy and nursing care for first two weeks, three times a week, meaning about six times in two weeks. And then two weeks after surgery, they would come and see me in the office. We’ll take a look at the incision, get some x-rays, and then they will progress to outpatient therapy. For the most part, patients by six weeks feel fairly good and they can almost return to, I would say 50%, 70% of their activity level. And then hopefully, by three months, they will be back to where they were, but better.
Amanda Wilde (Host): Wow. That seems like a very short recovery time. Also, it’s nice that you walk patients through exactly what to expect each stage of the process.
Dr Jason Wong: Yeah. The first two weeks is the hardest because the pain is there. The leg is swollen. It’s a new knee or a new hip. But the visiting nurse, they are a group of people. They worked together for a while already. So they were able to navigate with the patients about expectations, and, for example, like when can they shower? How is the incision looking compared to other people? And the truth is whenever a question arises the patient’s not comfortable with, they’ll ask the nurse and if the nurse is not comfortable, they would just give me a call. And despite they’re home, they’re not home alone. They’re home with support.
Amanda Wilde (Host): Yeah. We talked about different stages of the process of identifying the problem, doing the surgery and recovery. What do you like most about the work you do as an orthopedic surgeon at Maimonides?
Dr Jason Wong: I like my job at Maimonides, mainly because I think patients when they have this severe arthritis, they really can’t walk well. They are not able to spend time with their grandchild or hold them or they aren’t able to do stairs. They can’t even go on a trip with them. I have patients who were not able to go back to China because they just can’t navigate the system with the pain in their hips and knees. And so, what I like the most is that when we perform this kind of surgery, to me or to most of us, it’s like two hours of work, but you’re able to change the quality of life of the patients a lot after the surgery, if everything goes well. And that’s why I love to be an orthopedic surgeon because I’m able to change the quality of life or improve the quality of life of patients in a relatively quick manner.
Amanda Wilde (Host): Is there anything else you’d like to share about robots or joint replacement surgery?
Dr Jason Wong: I think I tried to get my point across earlier, that the robotic surgery is not that like I programmed something and I just sit down on my couch and watch the robot do the surgery for the patients. I think the live feedback and the pre-op planning is crucial to the success of surgery. And, bear in mind that despite there’s a robotic arm, my hand is on that arm. So I just want people to understand that the surgeon is actively doing the surgery, but then we’re doing it with the robotic guidance in a much more accurate manner than we were able to do before.
Amanda Wilde (Host): And you can do really specific and individual treatment plans for each patient.
Dr Jason Wong: Yes. That’s absolutely correct.
Amanda Wilde (Host): And that is the best. This conversation has been so beneficial in making clear how robotic surgeries you’re doing help recovery and quality of life for the many of us who do need hip and knee replacements. I appreciate you sharing your time and knowledge today, Dr. Wong.
Dr Jason Wong: Oh, thanks for having me.
Amanda Wilde (Host): If you’d like to make an appointment to see Dr. Jason Wong at Maimonides Bone and Joint Center located on Bay Parkway in Brooklyn, you can go to the website orthobrooklyn.com or call (718) 283-7400. This has been Maimo Med Talk. I’m Amanda Wilde. Stay well